UTI Treatment Online with a General Practitioner (GP) or Nurse Practitioner (NP)
-topaz-upscale-1.3x.jpeg)
UTIs are common, but they matter
If you’ve had a urinary tract infection (UTI), you know how miserable it feels. That constant urge to pee, the burning, the discomfort in your lower belly — it’s frustrating, painful, and exhausting. UTIs are one of the most common infections in women; in fact, over 1 in 2 women will experience at least one in their lifetime.
The good news: UTIs are straightforward to diagnose and treat. The better news: you don’t always need to visit a clinic in person. With telehealth UTI treatment, an Australian General Practitioner (GP) or Nurse Practitioner (NP) can:
- Assess your symptoms
- Prescribe antibiotics if appropriate
- Send an online UTI prescription directly to your pharmacy
- Arrange further tests if needed
This means you get help faster, without the waiting room shuffle.
Important: UTIs are usually minor, but they can become serious if ignored. If you have fever, flank/back pain, vomiting, are pregnant, immunocompromised, or feel very unwell — please seek in-person care or call 000.
Understanding UTIs: what’s actually happening?
A UTI occurs when bacteria (most commonly E. coli, which normally lives in the gut) enter the urinary tract — the urethra, bladder, ureters, or kidneys.
Types of UTIs
- Cystitis (bladder infection) — the most common, causing burning and frequency.
- Urethritis (urethra infection) — often linked with STIs but can cause similar discomfort.
- Pyelonephritis (kidney infection) — more serious, with fever, back pain, and sometimes nausea.
Why women are more affected
Women have a shorter urethra, which makes it easier for bacteria to reach the bladder. Hormonal changes (e.g. menopause), sexual activity, pregnancy, and anatomy also play a role.
Men, children, and older adults can get UTIs, but they’re less common and often considered “complicated” — which usually means face-to-face care is best.
-topaz-upscale-1.3x.jpeg)

Symptoms: what’s normal and what’s a red flag
Typical UTI symptoms include:
- Burning or stinging when passing urine
- Needing to pee more often, but with little output
- Cloudy, smelly, or bloody urine
- Lower abdominal pressure or pelvic discomfort
Red flag symptoms (see a doctor urgently):
- Fever, chills, or sweats
- Nausea or vomiting
- Pain in the back, side, or under the ribs
- Feeling very unwell, faint, or confused (especially in older adults)
If these are present, it may be a kidney infection — telehealth isn’t enough. Head to urgent care.
What telehealth can (and can’t) do for UTIs
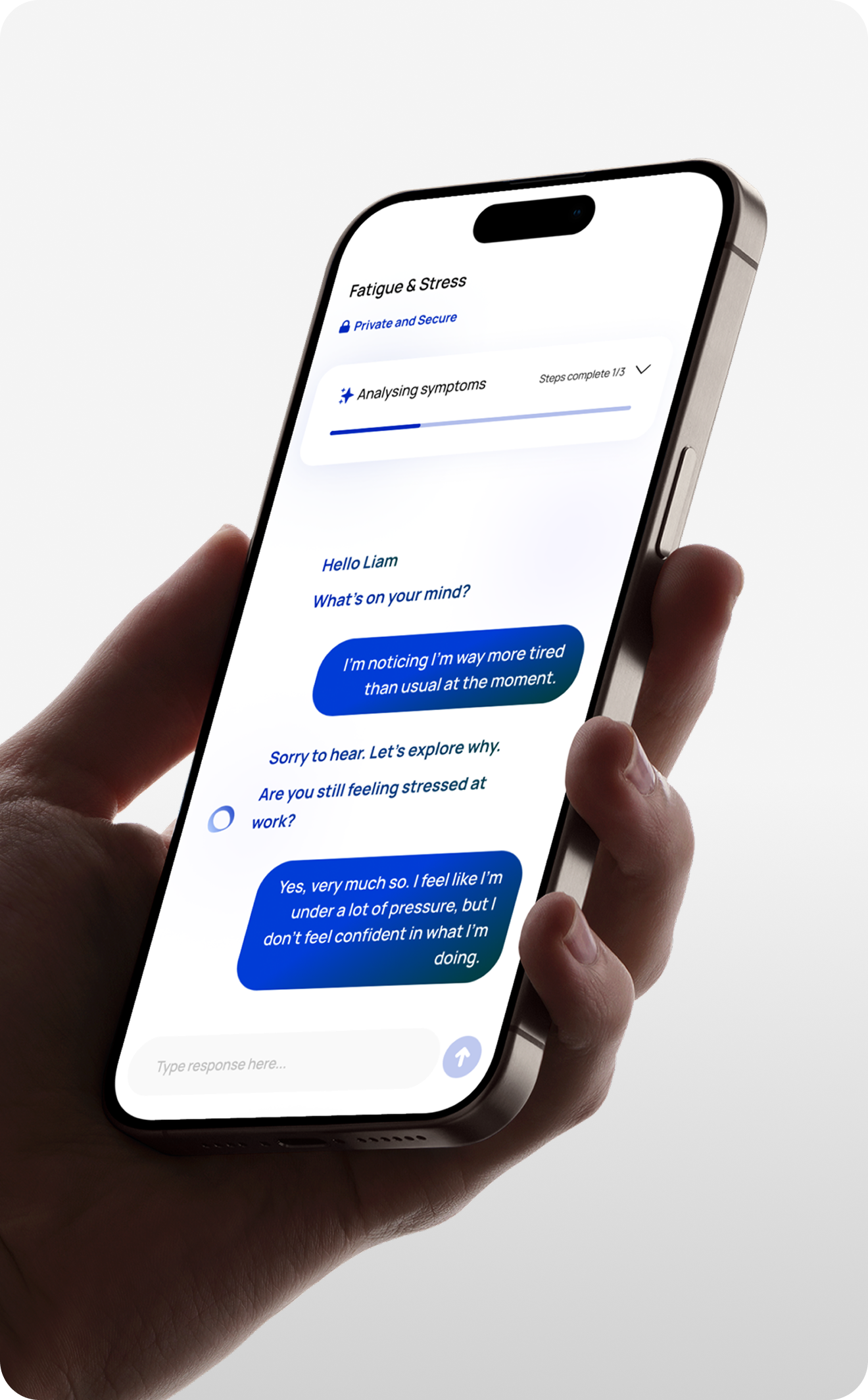
At Abby Health, here’s what happens in a telehealth consult for a UTI:
- History taking — your GP/NP asks about symptoms, duration, past UTIs, allergies, other health conditions.
- Assessment — based on your history, they determine if it’s likely an uncomplicated UTI.
- Treatment plan — this might include antibiotics, self-care advice, or a referral for further tests.
- Prescription — if antibiotics are appropriate, your GP/NP sends an eScript (electronic prescription) to your phone or directly to a pharmacy.
- Safety-netting — you’re given clear instructions on when to follow up, what to watch for, and when to escalate care.
What telehealth can’t do
- Perform a physical exam (sometimes needed for recurrent/complicated cases)
- Provide IV antibiotics (needed for kidney infections)
- Replace urgent hospital care
Telehealth is ideal for straightforward UTIs in otherwise healthy adults.
Antibiotics: how online prescriptions work
Yes, you can get antibiotics online in Australia. Here’s how:
- eScripts are government-supported: They are secure, trackable, and widely accepted across pharmacies.
- Not every case needs antibiotics: For mild UTIs, sometimes pain relief and hydration are enough. Your GP/NP will guide you based on best practice and Australian guidelines.
- Common antibiotics prescribed: Trimethoprim, nitrofurantoin, or cephalexin (always tailored to your history and allergies).
Most people feel significant relief within 24–48 hours of starting antibiotics. If not, it’s important to follow up — resistant bacteria or another condition may be the cause.
Ready to Feel Better?

Prevention: stopping UTIs before they start
Recurrent UTIs are frustrating. Prevention strategies your GP/NP may discuss include:
- Hydration: Drinking plenty of water dilutes urine and helps flush bacteria.
- Don’t delay urination: Empty your bladder when you feel the urge.
- After sex: Urinating post-sex helps clear bacteria from the urethra.
- Avoid irritants: Perfumed soaps, bubble baths, and sprays can disrupt natural flora.
- Clothing choices: Cotton underwear and breathable fabrics can reduce irritation.
- Prophylaxis: In select recurrent cases, your GP may discuss preventive antibiotics or specialist referral.
If UTIs keep coming back, pathology tests can be arranged via telehealth to rule out underlying conditions (e.g., kidney stones, diabetes, anatomical differences).
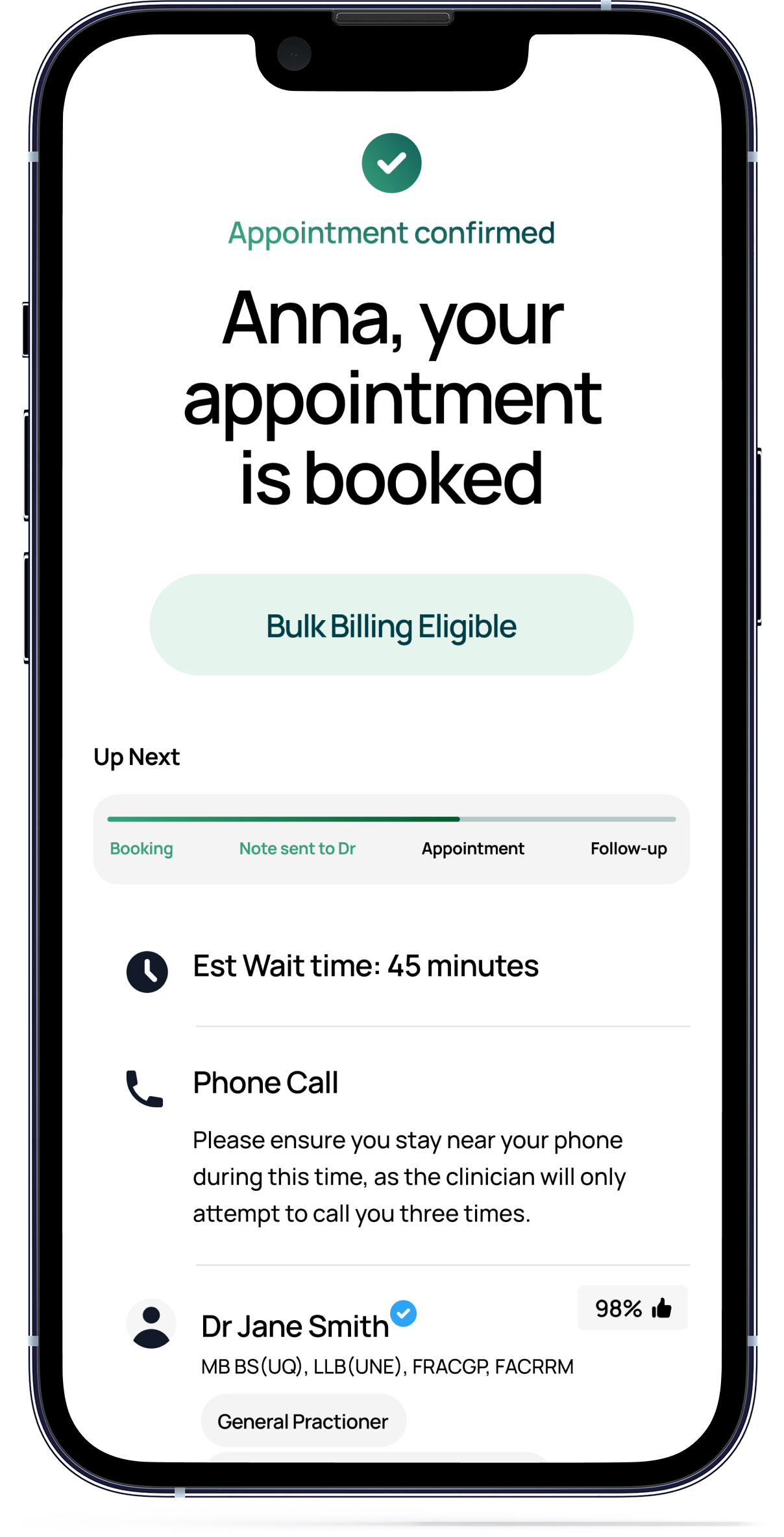
Why choose Abby Health for UTI treatment?
- Bulk-billed consults (no gap fees with Medicare)
- Experienced women’s health GPs and NPs
- eScripts direct to pharmacy — usually same-day treatment
- Continuity of care — follow-up, referrals, and broader women’s health support
Abby Health is designed for long-term care on demand — not just quick scripts, but ongoing GP/NP support when you need it.
Editorial Standards
Notice something that doesn’t look right? Let us know at support@abbyhealth.app
- Healthdirect — Urinary tract infection (UTI)
- Healthdirect — Cystitis
- Healthdirect — Kidney Infection
- Healthdirect — Urinary system
- NSW Health — UTI FAQs for the Community
- NSW Health — UTI Treatment at Pharmacies (Community Info)
- NSW Health — Pharmacist Practice Standards for UTI Antibiotics (PDF)
- NSW Health — UTI Treatment for Pharmacists
- NSW Clinical Excellence Commission — Antimicrobial Stewardship
- ACI Health NSW — UTI in Women Factsheet